Wisdom Teeth
Why do we get wisdom teeth?
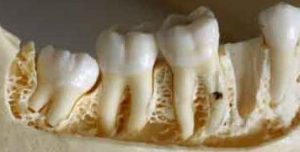
Wisdom teeth or third molars are your four hindmost molars that erupt usually by the age of 18-20 years of age. It is believed that wisdom teeth were developed as a result of the wear on our teeth from our ancestors. Their diet of leaves, grains, seeds and nuts required more chewing power which led to excessive wear on the posterior teeth. Anthropologists have studied the human jaw in order to learn about the evolution of our diets.

Are my wisdom teeth necessary?
According to the American Association of Oral and Maxillofacial Surgeons, approximately 65-80% of adults have had 1 or more wisdom teeth removed. Not everyone has wisdom teeth and some may only get 1 or more. Like our ancestors who developed a third set of molars with evolution, we may see a decline in development as they are no longer needed in our diets today. It is recommended to have your wisdom teeth removed if they cause pain, periodontal (gum) issues, or bite issues. Some people have adequate space for full eruption of their wisdom teeth (third molars) without posing any issues at all. When aligned properly, your wisdom teeth will provide more chewing surfaces and can aid in digestion.
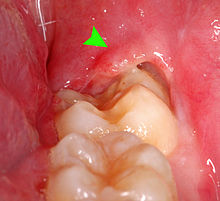
This photo from Wikipedia illustrates a partially erupted wisdom tooth that has created a periodontal issue. When a tooth is partially erupted, the gum tissue cannot completely be removed from the tooth and bacteria and debris can create an infection under the tissue.
How do I know if I need to have my wisdom teeth removed?
Your dentist will recommend your wisdom teeth be removed if they do not fully erupt from the gums or do not erupt at all. Some symptoms you may experience are:
–Persistent pain; you will experience persistent pain or pressure in the back of your jaw where the wisdom teeth will erupt

–Stiffness in your jaw; caused by the shifting of surrounding teeth as the wisdom teeth begin to erupt.
–Consistently irritated gums; this is also known as pericoronitis. It occurs when plaque and bacteria becomes trapped under the gum tissue surrounding the partially erupted tooth/teeth. This creates an infection that re-occurs until the tooth is removed.
If you are experiencing these symptoms it is important to keep the area as clean as possible until you are able to have the teeth removed. Brushing, flossing and warm salt water rinses can help reduce bacteria and plaque buildup. An over-the-counter anti-inflammatory such as Motrin can help reduce the inflammation in the area. Warm moist compresses on the outside of the mouth help relax the muscle tissues and reduce soreness. Stick to a soft diet to reduce over use of the jaw.
Photo from identalhub.com
Who removes wisdom teeth?
Your general dentist may extract wisdom teeth if they are simple extractions. However, most general dentists refer wisdom tooth extractions to an Oral Surgeon. Oral surgeons have the ability to sedate the patient, which provides more comfort to the patient for difficult extractions that may be a longer procedure. If it is recommended to have your wisdom teeth removed and the treatment is ignored you will put yourself at risk for consistent infections. When impacted, not fully erupted, it is nearly impossible to properly clean these teeth. Having a surplus of harmful bacteria in your mouth leads to an increase in tooth decay as well as reoccurring pericoronitis. It is always best to remove wisdom teeth as soon as it is recommended. As the teeth develop and fully form they may pose a risk on the nerves surrounding them which lead to more difficulty during surgery and greater post-operative risks including permanent paralysis from nerve damage in the lower jaw. This is also more costly.